Medically Not Yet Explained Symptoms

About this Priority Setting Partnership
Medically Not Yet Explained Symptoms represent up to 10-30% of presentations in general medicine settings. They can include fatigue, pain, dizziness, irritable bowel syndrome, and functional neurological symptoms.
The focus of research on Medically Not Yet Explained Symptoms is often on particular subsets of symptoms, such as chronic pain, chronic fatigue, irritable bowel syndrome, or dizziness, but it lacks a comprehensive view. This has ramifications for patients who visit different clinics for their various symptoms, without sustained improvement.
The Medically Not Yet Explained Symptoms PSP was established in 2020 to support patients, carers and healthcare professionals in the UK and in the Netherlands in the development of a research agenda with patient knowledge, experience and preferences as the frame of reference.
This Anglo-Dutch partnership also aimed to enable exploration of international and intercultural differences that might be of interest for future development of services and the co-design of research to develop better treatment and care.
The Medically Not Yet Explained Symptoms PSP UK Top 10 was published in September 2021.
Top 10 priorities Netherlands
- What can be done to ensure that people with MNYES are correctly diagnosed and appropriately treated more quickly?
Hoe kan ervoor gezorgd worden dat iemand met medisch niet voldoende verklaarde klachten sneller de juiste diagnose en passende zorg krijgt? - Which factors play a role in the development of MNYES?
Welke factoren spelen een rol bij het ontstaan van medisch niet voldoende verklaarde klachten? - Which treatment works best for which individual with MNYES?
Welke behandeling werkt het beste voor welk individu met medisch niet voldoende verklaarde klachten? - What needs to happen to help people with MNYES understand their symptoms?
Wat moet er gebeuren om mensen die medisch niet voldoende verklaarde klachten hebben hun eigen klachten te helpen begrijpen? - Some people experience great difficulty with adjusting to their MNYES; others experience less difficulty; why does this differ and what lessons can be learned from these differences?
Sommige mensen hebben veel moeite om met hun medisch niet voldoende verklaarde klachten om te gaan; andere mensen hebben daar minder moeite mee: wat maakt het verschil en wat kunnen we daar van leren? - What support do people who are close to someone with MNYES (family, friends) need?
Welke ondersteuning hebben naastbetrokkenen (familie, vrienden) van mensen met medisch niet voldoende verklaarde klachten nodig? - What can we learn from the treatment-related experiences of MNYES-professionals and how can we use these experiences to improve treatment?
Wat kunnen we leren van de behandelervaringen van zorgverleners van patiënten met medisch niet voldoende verklaarde klachten en hoe kunnen we die ervaringen inzetten om de behandeling te verbeteren? - What is the role of trauma or other adverse childhood life-events in the development of MNYES?
Wat is de rol van trauma’s of andere nare levensgebeurtenissen in de kindertijd bij het ontstaan van medisch niet voldoende verklaarde klachten? - What can be done to reduce the negative feelings (e.g., hopelessness, frustration) that some people (patients as well as health care professionals and others involved) have with regards to MNYES?
Wat kan er gedaan worden om de negatieve gevoelens (bijvoorbeeld: hopeloosheid en frustratie) te verminderen die mensen, zowel patiënten als zorgverleners en andere betrokkenen, hebben als gevolg van medisch niet voldoende verklaarde klachten? - What are the possible interventions which could prevent MNYES?
Wat zijn mogelijk preventieve interventies ter voorkoming van medisch niet voldoende verklaarde klachten?
The following questions were also discussed and put in order of priority at the workshop:
- What issues are relevant in the workplace of people with MNYES and how can these be improved (e.g. adjusting working conditions or finding suitable work)?
Welke kwesties spelen er in de werksituatie van mensen met medisch niet voldoende verklaarde klachten en hoe kan dat verbeterd worden (bijv. aanpassen van de werkomstandigheden of het vinden van passend werk)? - Why do multiple conditions with MNYES often occur together in the same person?
Hoe komt het dat verschillende aandoeningen met medisch niet voldoende verklaarde klachten vaak tegelijkertijd bij één persoon voor komen? - Which symptoms are most often reported by people with MNYES and which symptoms should future research focus on?
Van welke symptomen hebben mensen met medisch niet voldoende verklaarde klachten het meeste last en op welke symptomen moet toekomstig wetenschappelijk onderzoek zich richten? - Why does the severity of MNYES fluctuate without a clear reason?
Waarom wisselt bij veel mensen met medisch niet voldoende verklaarde klachten de ernst van symptomen, zonder dat daar een duidelijke reden voor te vinden is? - What information/education should be provided and to whom in order to help people (and their carers) with MNYES?
Welke voorlichting moet aan wie gegeven worden ter preventie van medisch niet voldoende verklaarde klachten? - Which terminology is best for MNYES?
Welke benaming kan het beste gebruikt worden voor medisch niet voldoende verklaarde klachten? - How often do people get diagnosed with MNYES?
Hoe vaak wordt de diagnose ‘medisch niet voldoende verklaarde klachten’ gesteld? - How often is the diagnosis of MNYES missed?
Hoe vaak wordt de diagnose ‘medisch niet voldoende verklaarde klachten’ gemist?
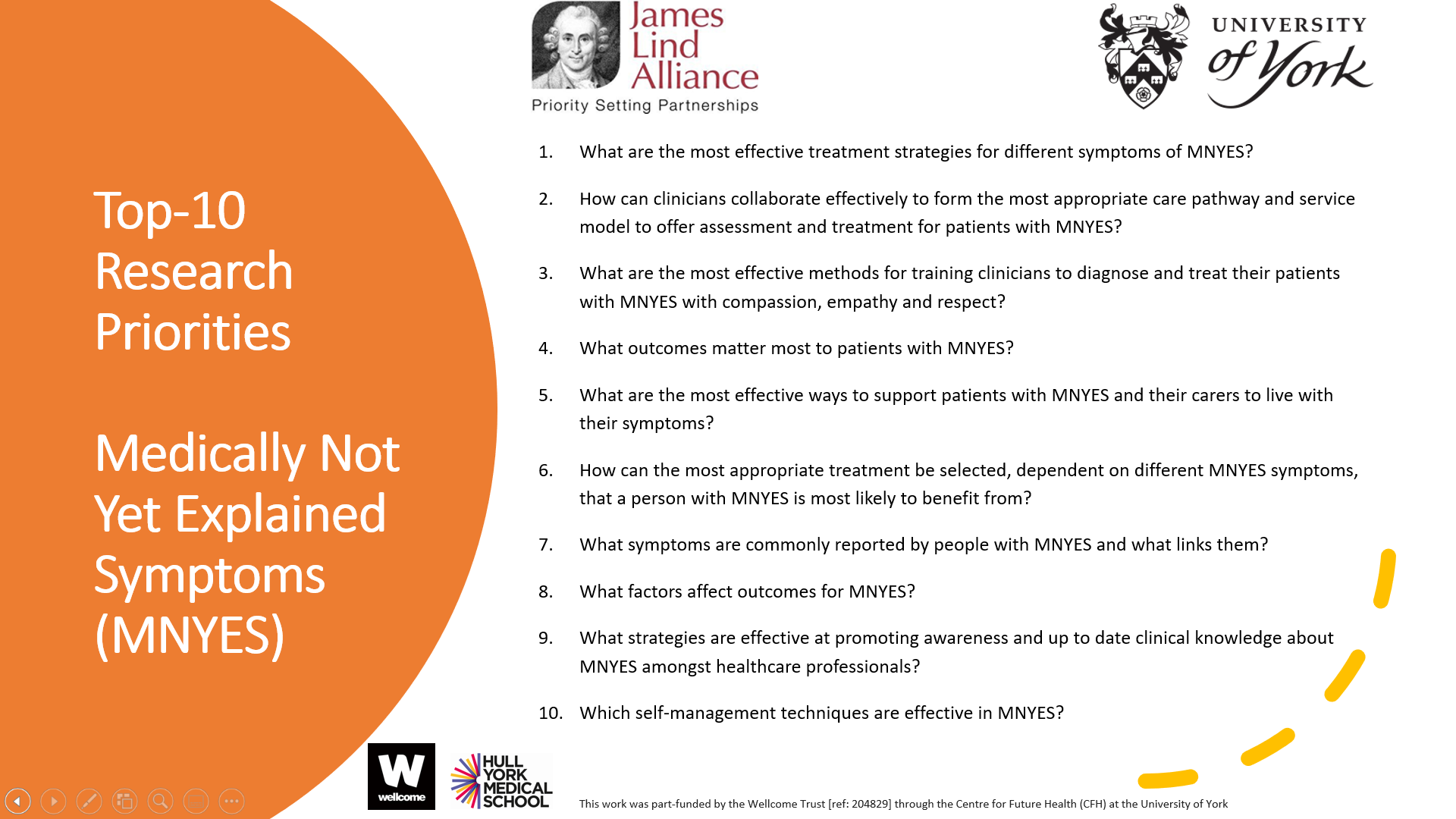
Top 10 priorities UK
- What are the most effective treatment strategies for different symptoms of MNYES?
- How can clinicians collaborate effectively to form the most appropriate care pathway and service model to offer assessment and treatment for patients with MNYES?
- What are the most effective methods for training clinicians to diagnose and treat their patients with MNYES with compassion, empathy and respect?
- What outcomes matter most to patients with MNYES?
- What are the most effective ways to support patients with MNYES and their carers to live with their symptoms?
- How can the most appropriate treatment be selected, dependent on different MNYES symptoms, that a person with MNYES is most likely to benefit from?
- What symptoms are commonly reported by people with MNYES and what links them?
- What factors affect outcomes for MNYES?
- What strategies are effective at promoting awareness and up to date clinical knowledge about MNYES amongst healthcare professionals?
- Which self-management techniques are effective in MNYES?
The following questions were also discussed and put in order of priority at the workshop:
- What is the relationship between mental health problems and MNYES?
- What is the relationship over time between MNYES and known medical conditions and does that suggest some shared pathological process?
- What is the best practice to offer optimal care for patients with MNYES?
- What are current clinical attitudes and levels of knowledge about MNYES?
- What are the most effective physical treatments for different symptoms of MNYES?
- What are the most effective psychological treatments for different symptoms of MNYES?
- Why do symptoms of MNYES fluctuate?
Document downloads
For full details of all of the questions identified by this PSP, please see the document below.